Are skin cancer checks part of your consultation? Jennifer Byrne explains why they should be, and the important role skin practitioners play in early skin cancer detection.

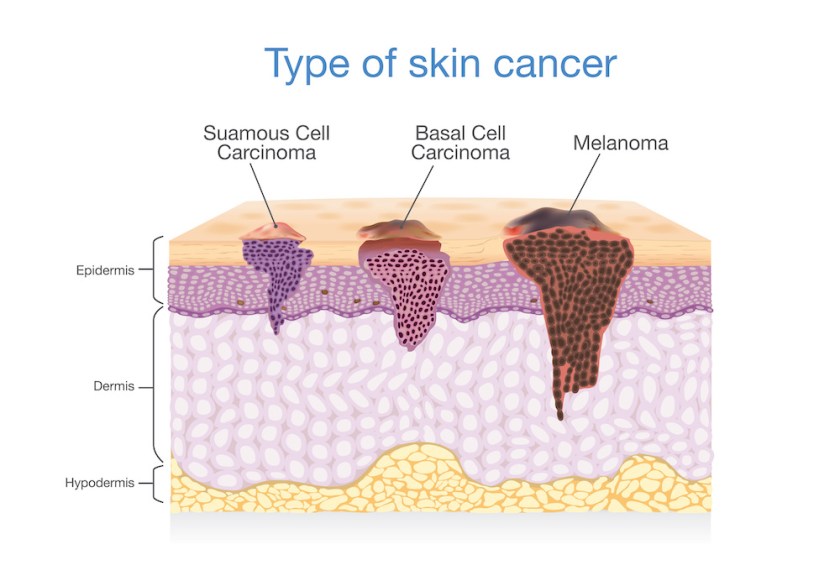
In Australia, we have one of the highest prevalence rates of skin cancer in the world. Two out of three Australians will be diagnosed with skin cancer in their lifetime. The two most common skin cancers are non-melanomas including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). The cost to the healthcare system is considerable with over 700 million dollars in health care funding associated with hospitalisations due to non-melanoma skin cancer. According to medicare records more than 100 million treatments are performed each year or approximately 3000 treatments per day. Melanoma is the third most common skin cancer and is the most life threatening. Approximately 16,000 individuals are diagnosed each year, it is the most common cancer affecting young people from 20-39 years of age. 1,2,3
Why should people have a skin check before skin treatments?
Skin cancer is often thought of as pigmented lesions or obvious skin lumps and bumps. While skin cancers often do present that way, skin cancer and its precursor lesions can also present in many different ways. For those that are not familiar with assessing and treating skin cancer it can be hard to distinguish between skin cancers from lesions that clients may be commonly seeking our assistance to treat for cosmetic concerns.
There are published cases where as yet undiagnosed skin cancers have been treated over unknowingly or diagnosis has been delayed as markers usually used to monitor or detect possible skin malignancy have been altered by treatments. While light based procedures are often discussed for potential harm it does have to be highlighted that any therapy particularly energy based that can alter, damage or partially remove vascular or pigmented lesions may be of equal concern.
Case Study : What can go wrong?
The case below, provided with consent from the client and clinic where treated highlights how easy it could be to miss skin cancer. In the case presented it was detected before treatment as the practice this client presented to has a Dermal Clinician and Nurse Practitioner with further training in dermoscopy which is used as a routine aspect of their skin assessment.
A 47 year-old assigned female at birth presented with concerns about actinic (sun) damage, and redness associated with Rosacea. The client had a personal history of non-melanoma skin cancer. To an untrained eye or for those that rely on using the naked eye in skin examinations this skin looks very typical of a rosacea skin. The skin had no reported pruritis or irritation by the client but did comment that the redness on her skin had been present for several years and had appeared to be worsening over the last 12 months. Otherwise her skin could be a bit dry and flaky. Can you see any area that may be of concern for further evaluation?

During skin assessment the clinicians identified two areas of concern for further evaluation; one on the left check and the other on the right upper forehead. This client was referred to a dermatologist for further investigation before any further therapy would be provided. Pathology returned a diagnosis of basal cell carcinoma (BCC) on the left cheek and a focal intra-epidermal carcinoma (IEC) on the right forehead. This patient was then referred to a plastic surgeon for removal of the BCC and treatment by the nurse practitioner using PDT to remove IEC and solar keratoses before further treatment could commence for her concerns of Rosacea. The client also was referred for a full body skin check.
Who can and who cannot detect skin cancers?
Population based skin screening for skin cancer is currently not recommended like it is for other cancers due to a lack of evidence it would reduce mortality or morbidity 4,5. Due to the prevalence of skin cancer, it is recommended that we should all know how to monitor our own skin for changes in order to seek prompt medically provided skin checks if there are concerns. This is termed opportunistic skin screening.
As skin health professionals that often see our clients regularly and over long periods of time we have a role to play in skin screening and observing for skin changes. Through being well educated in skin cancer risk and understanding the medical pathways for diagnosis and treatment we can assist with early detection of skin cancer. This may assist to reduce mortality as well as morbidity such as more significant scarring that can result from delayed diagnosis requiring more extensive surgical removal.
While skin health professionals can monitor the skin for skin changes and should be educated about signs of possible skin cancers, we can’t diagnose them. Skin cancer is diagnosed through a biopsy and referral to pathology for histological review. This is looking at cells under a microscope. Those tests are ordered by medical professionals. Unless we have specialised training in dermoscopy and skin cancer medicine, it is also very difficult to determine that a skin lesion is definitely benign. Therefore skin checks should be performed by those with specific training before proceeding with therapies that can remove markers in the skin used to monitor for skin malignancy.
Who can provide skin checks?
Sun Smart Australia has an information sheet that is used to guide the public with advice on who can perform skin checks and questions to ask. As a skin health professional, you may also receive questions or want to know who can assist with skin checks:
Dermoscopists – These are often nurses or dermal clinicians with post-graduate qualifications in the field of dermoscopy. They assist with education about skin cancer risk, performing full-body skin checks, and digital imaging of lesions for surveillance purposes. They will provide a report and referral if any lesions require medical review or follow-up.
Skin Cancer GPs – Many general practitioners perform opportunistic skin cancer screenings as part of their routine practice. There are also general practitioners who have undertaken significant further education in the assessment, diagnosis and management of skin cancer. The Skin Cancer College of Australasia accredits skin cancer doctors and also provides a locator service to assist with finding an accredited skin cancer GP.
Dermatologists – A dermatologist is a medical professional who has undertaken an extra four years of specialist training after their medical degree in the assessment, diagnosis and management of up to 3000 disorders and diseases that affect the skin, hair, and nails. Usually, you will require a referral to see a dermatologist and they work with other medical specialties such as plastic surgeons, cancer surgeons and radiation specialists when required.
Why are skin screenings not part of consultations now and how can we improve this?
Skin cancer screenings are not currently part of skin consultations for a few reasons.
- The skin health professional may not be aware of the potential harm that can arise from not checking the skin.
- Concerns that if you refer to a medical professional you may lose the client particulary if they provide cosmetic medical procedures.
- Concerns that the client may refuse to get a skin check if you mandate it and go some-where else for their services.
What can we do about this and what is best practice?
Education and networking can improve patient safety in providing skin services. There are a few ways to increase your knowledge and skill set in monitoring for skin cancer depending on your current qualifications and clinical setting.
The Skin Cancer College of Australasia recently developed introductory training modules for anyone that works with or sees skin regularly including beauty therapists and hairdressers. As well as for medical professionals, nurses, and allied health professionals including dermal clinicians that are new to the field of skin cancer. From there, depending on your background you may be able to complete further advanced training. This applies to allied health professionals including dermal clinicians, nurses, and medical professionals.
Obtaining more extensive and formalised education such as a degree in performing advanced skin therapies is important to improve patient safety. These formalised programs will have extended training in skin biology, dermatological conditions as well as risk assessment and prevention to perform therapies, how to form referral networks or integrate with other health professionals for example.
The Royal College of General Practitioners has published a stratified risk rating and protocol for skin checks in primary practice. This is a tool that can be used by skin health professionals to support educating clients as well as when making decisions regarding performing procedures that involve possible removal of markers for skin cancer monitoring. At the current time there is no guideline specific to skin health professionals however the Australian Society of Dermal Clinicians has initiated a working group with advisory from representatives from Dermatology and Skin Cancer Medicine as expert advisory for the development of a guidance document in 2023.
Best practice at this time would be to obtain a medically provided skin check with a statement that the lesion is definitively benign before treatment including test patching proceeds. As well as educating patients that treatments can remove markers that may be used to monitor the skin in the future for changes and how this should be handled. For high risk clients with many pigmented lesions or at very high risk of cancer for the future we should consider other methods of addressing the concern that will not remove markers for skin surveillance.
Jennifer Byrne is the Chair person of the Australian Society of Dermal Clinicians as well as a lecturer and the Clinical Coordinator for dermal science in the College of Health & Biomedicine at Victoria University.
References
- Cancer Council. Skin cancer incidence and mortality [Version URL: https://wiki.cancer.org.au/skincancerstats_mw/index.php?title=Skin_cancer_incidence_and_mortality&oldid=802, cited 2023 Mar 4]. Available from: https://wiki.cancer.org.au/skincancerstats/Skin_cancer_incidence_and_mortality.
- Cancer Council Australia. Skin Cancer Statistics and Issues. Sydney: Cancer Council Australia. Available from: http://wiki.cancer.org.au/skincancerstats/
- Cancer Council. Skin cancer types [Version URL: https://wiki.cancer.org.au/skincancerstats_mw/index.php?title=Skin_cancer_types&oldid=806, cited 2023 Mar 4]. Available from: https://wiki.cancer.org.au/skincancerstats/Skin_cancer_types. In: Cancer Council Australia. Skin Cancer Statistics and Issues. Sydney: Cancer Council Australia. Available from: http://wiki.cancer.org.au/skincancerstats/
- https://www.health.gov.au/sites/default/files/documents/2019/09/skin-cancer-screening-position-statement.pdf
- Janda. M., Olsen. C., Mar. V. & Cust. A. (2022). Early detection of skin cancer in Australia – current approaches and new opportunities. Public Health Research & Practice. Available from https://www.phrp.com.au/issues/march-2022-volume-32-issue-1/early-detection-of-skin-cancer-in-australia/
This article originally appeared in SPA+CLINIC 93.
Read SPA+CLINIC’s Latest Issue Here:
There are 5 ways you can catch up with SPA+CLINIC
- Our quarterly print magazine, delivered to your door. Subscribe here.
- Our website, which is updated daily with its own completely unique content and breaking news.
- Our weekly newsletter – free to your inbox! Subscribe here.
- Our digital magazine – click here to view previous issues.
- Our social media – see daily updates on our Instagram, Facebook & Linkedin




